 Conversation about BMI goes public
Last week, national publications such as the Huffington Post reported that body mass index (BMI) may not be the best measure of obesity. Obesity medicine clinicians have long utilized other means to measure and classify obesity, but this article represents a small shift in the public mindset. The author calls BMI an "unreliable metric" for diagnosing chronic diseases associated with weight, and points out that health insurance companies use BMI to calculate "financial discounts or penalties to policy holders." Read the full article in the Huffington Post. 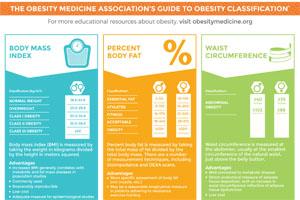 OMA offers a free, printable poster explaining the three most common methods of classifying obesity. Download and print our "classifying obesity" poster to hang in your patient exam rooms. |
Our favorites from #ILoveObesityMedicine
Our favorite post on social media from last week's #ILoveObesityMedicine campaign came from Dr. Michael G. Knight: #ILoveObesityMedicine because I love the look on my patients' faces when they're losing weight and living their best life!Thank you, Dr. Knight, for your dedication to improving your patients' health!
|
Designate OMA as your primary medical specialty society
OMA currently holds one seat in the American Medical Association's (AMA) House of Delegates. Having a seat means we have a voice within the AMA, and we can influence policy, introduce initiatives, and ensure that AMA keeps talking about obesity. Help us strengthen our voice by designating OMA as your primary specialty society. For every 1,000 people who choose OMA as their primary specialty society, we're allowed one additional delegate in the House of Delegates.
|
Obesity Treatment Foundation
|
 Meet Dr. Cherie Vaz, winner of the $7,500 pilot grant in 2015
Dr. Cherie Vaz is an assistant professor of medicine at Temple University, Lewis Katz School of Medicine, where she practices endocrinology and obesity medicine. She currently conducts clinical and translational research at Temple University in the fields of obesity, type 2 diabetes and metabolic syndrome. The grant from the Obesity Treatment Foundation will support a study evaluating the use of smart technology as a weight-loss tool. Dr. Vaz is a member of the Obesity Medicine Association, is a diplomate of the American Board of Obesity Medicine, and is board-certified by the American Board of Internal Medicine and Endocrinology. She currently treats about 50 patients per week for obesity. Dr. Vaz's winning grant proposal is titled, "Non-exercise activity thermogenesis and heart rate variability in patients with obesity." |
 |
Quantifying the proportion of deaths due to BMI- and waist-circumference-defined obesity
Tanama, S. K., et al. Obesity, 2016.
Obesity is most commonly defined using body mass index (BMI); however, it may not be the best measure to identify high-risk adiposity. Dual-energy X-ray absorptiometry and bioelectrical impedance analysis can reliably estimate total body fat; however, they are not realistic to use in large-scale populations. There have been many studies comparing BMI to waist circumference, weight-hip ratio, and waist-height ratio in relation to health risk, but there has not been a consensus for the other measures being superior to BMI. This study of more than 41,000 participants was conducted to determine the risk of mortality associated with BMI and waist circumference and to quantify the deaths attributable to combinations of BMI and waist circumference (WC). The study found that there was an increased risk of all-cause and cardiovascular disease mortality in participants with a normal BMI and obese WC compared to those with normal BMI and normal WC. The proportion of all-cause and CVD mortality attributable to obesity defined using WC, or using BMI and/or WC, was higher compared to obesity defined using BMI alone. The authors suggest that targeting BMI alone misses many individuals who are at increased risk of mortality due to their WC. View article
|
Higher compared with lower dietary protein during an energy deficit combined with intense exercise promotes greater lean mass gain and fat mass loss: A randomized trial
Longland, T. M., et al. AJCN, 2016.
Increased dietary protein combined with exercise is helpful in preserving lean body mass during an energy deficit. A study was conducted to test whether different amounts of protein combined with resistance and high-intensity interval training six days per week affected body composition during a hypocaloric diet (40 percent deficit). The four-week study found that the men who were consuming higher protein diets (2.4 g/kg/day) actually increased their lean body mass (+1.2 kg) compared to baseline, while the lower protein group (1.2g/kg/day) did not have a change in lean body mass. Whey protein was supplemented post exercise to promote lean mass retention. Both groups significantly decreased fat mass after the intervention, with the higher-protein group having greater losses in fat mass than the lower-protein group. These results suggest that it is possible to lose weight and fat mass and increase lean body mass with an intensive dietary and training regimen. View article
|
|
|
|
Executive Director
Sponsorships and Exhibits Manager
Operations Manager
Education Coordinator
Communication Manager
Executive Director of the Obesity Treatment Foundation
|
|
101 University Blvd.,
Suite 330
Denver, CO 80206
|
|
|
Incretin therapies: Highlighting common features and differences in the modes of action of glucagon-like peptide-1 receptor agonists and dipeptidyl peptidase-4 inhibitors
Nauck, M. Diabetes, Obesity and Metabolism, 2016.
Over the last few years, incretin therapies, such as glucagon-like peptide-1 (GLP-1) receptor agonists and dipeptidyl peptidase-4 (DPP-4) inhibitors, have become popular approaches to the treatment of type 2 diabetes as well as obesity. Incretins not only stimulate insulin secretion, but are also associated with additional non-glycemic benefits such as weight loss and improvements in beta-cell function and cardiovascular risk markers. Many physicians use incretins to tailor treatment plans, given their beneficial properties. This review outlines the commonalities and differences among incretin-based therapies and gives guidance regarding agents most suitable for treating type 2 diabetes in individual patients. View article
|
 |

This spring, we're headed to lively San Francisco for Obesity Medicine 2016, your leading resource for certification exam review and the premiere source of education about managing an obesity medicine clinic, nutrition, and the comprehensive approach to obesity treatment. Earn up to 30.5 CME/CE and attend the courses that most interest you!* While you're there, don't miss all that San Francisco has to offer. Take a trip to Alcatraz for a taste of history, walk along the waterfront or the Golden Gate Bridge, or visit one of the city's many cultural districts. |
Review Course for the ABOM Exam
13.25 CME/CE | April 6-7
Helps prepare those planning to take the American Board of Obesity Medicine (ABOM) certification exam.
| Practice Management Essentials
6.5 CME/CE | April 6
Explains the best business practices for running an obesity medicine clinic, from setting up a practice to boosting patient retention.
|
|
Nutrition Course
6.75 CME/CE | April 7
Outlines the latest evidence-based findings about nutrition and helps you select appropriate nutrition plans for your patients.
| Spring Obesity Summit
17.25 CME/CE | April 8-10
Addresses topics related to current and emerging research, evidence-based treatment approaches, technologies, and practical methods used by obesity medicine clinicians.
|
|
|
*The Review Course for the ABOM Exam runs concurrently with Practice Management Essentials on Wednesday and the Nutrition Course on Thursday. Registration for the Review Course includes two days of class time, and switching between courses is not allowed.
|
 There are only two Obesity Medicine Basics courses left this winter. Don't miss your opportunity to either attend this introductory-level course or refer a colleague to attend and earn a $50 Amazon gift card*. Obesity Medicine Basics is worth up to 7 CME/CE hours and provides introductory-level training about the evaluation and treatment of patients affected by obesity. Learn more about this course. Course dates and cities:*For every person you refer who attends an Obesity Medicine Basics course in any city and lists you as the person who referred them, you'll earn a $50 Amazon gift card. |
|
|
|
The Obesity Medicine Association and the Obesity Treatment Foundation thank our 2016 Corporate Advisory Council members for their continuous support.
|
© 2016 Obesity Medicine Association. All rights reserved. Materials may not be reproduced, redistributed or translated without written permission. Advertising disclaimer: Under a policy approved by the OMA executive committee and exhibitor/advertiser review committee, commercial companies may apply to advertise in OMA publications. Approval does not imply endorsement or official recognition of particular products or services.
|
|
|
|